We are proud to announce a valuable addition to the widely-used LOINC clinical terminology standard. This addition is the LACE scale. It identifies patients who are at risk for readmission or death within thirty days of discharge.
This is of great import to hospitals in deciding whether and when it is safe and appropriate to discharge a patient. Readmission or death of a patient within thirty days of discharge is considered an “adverse event” and can result in a financial penalty to the hospital from Medicare as a provision of the Affordable Care Act. For the sakes of both the hospital and the patient, premature discharges are to be avoided.
LACE Explained
The acronym stands for the four factors that are considered in making this determination:
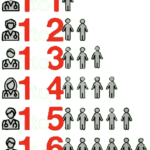
“L”: the length of stay of the admission
“A”: the acuity of the admission (emergency or elective)
“C”: co-morbidities (the Charlson Co-Morbidity Index)
“E”: the number of Emergency Department visits within the last 6 months
This tool is widely used by hospitals as part of the process of deciding when to discharge patients. We describe it in detail here.
In order to capture the result of the LACE assessment in an electronic health record (EHR), a clinical coding scheme is required. The two most popular for this purpose are Snomed and LOINC. We at Nurse Tech use LOINC for communicating with EHRs, enabling them to receive and store our nurse users’ assessments that now include LACE.
As a result of our submission to LOINC’s review process and with the permission of Dr. Carl Van Walraven, LACE’s author, LACE is now part (and, we claim, a valuable part) of an important electronic clinical terminology.
Thank you LOINC, Dr. Van Walraven, and Nurse Tech. And go nurses!